“The function, the very serious function of racism is distraction. It keeps you from doing your work. It keeps you explaining, over and over again, your reason for being. Somebody says you have no language and you spend twenty years proving that you do. Somebody says your head isn’t shaped properly so you have scientists working on the fact that it is. Somebody says you have no art, so you dredge that up. Somebody says you have no kingdoms, so you dredge that up. None of this is necessary. There will always be one more thing”.-Toni Morrison
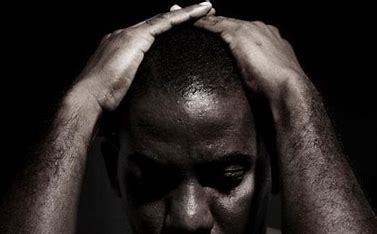
On May 1, 2023, a grisly murder unfolded within the confines of a New York Subway train, shattering the lives of those involved. Witnesses and video testimony recount the chilling moment when Jordan Neely, a 30-year-old homeless Black man battling mental illness, boarded the F train and unleashed his anguish: “I don’t have food, I don’t have a drink, I’m fed up.” Neely then went on to exclaim “I don’t mind going to jail and getting life in prison. I’m ready to die.” What followed was a disturbing display of violence as Daniel Penny, a white 24-year-old Marine veteran, and others restrained Neely in a chokehold for a reported 15 minutes until he succumbed to unconsciousness and death.
In the aftermath of this harrowing incident, countless questions have arisen, demanding answers. Was Daniel Penny’s response truly appropriate, and to what extent should Jordan Neely bear responsibility for his tragic demise? However, embedded within these discussions lies a profound and unsettling truth—the ultimate perpetrator accountable for Jordan Neely’s untimely death is none other than systemic racism itself.
Amidst the sorrow and despair, we must confront the stark reality of how anti-Black racism in mental health intertwines with catastrophic consequences, not only in isolated incidents but throughout our society. Mental illness, homelessness, racism, and poverty should never have conspired to bring about Jordan Neely’s demise. Yet, our collective failure to address these intersecting oppressions continues to perpetuate preventable tragedies for those who bear their weight. Jordan Neely’s death serves as a visceral reminder of the manifold ways in which the mental health system has failed Black individuals, revealing an urgent need to rectify the pervasive grip of anti-Black racism in mental health.
Sadly, the death of Jordan Neely represents merely one ghastly symptom of an insidious malady—systemic racism—that plagues the very heart of mental health care. Today, an overwhelming abundance of data illuminates the myriad ways in which anti-Black racism permeates the field of mental health, contributing to biased diagnoses, woefully inadequate treatment, and the cruel denial of access to essential mental health services.

Anti-Black racism in mental health manifests in various ways.
Moreover, any discussion of anti-Black racism’s manifestations in mental health would be incomplete without addressing how it impacts the brain, giving rise to troubling mental afflictions. As we have discussed previously, racial stressors contribute to increased allostatic load and weathering, impacting the brain and worsening health outcomes . Similarly, Psychiatric sciences have long acknowledged the fact that stress is causally implicated in an enormous range of mental disorders, referring to the “stress-diathesis model” of mental illness. This model incorporates the well-documented fact that chronic stressors, including poverty, political violence, and discrimination, intensify the likelihood of developing mental disorders ranging from depression to schizophrenia. Moreover, this chronic elevation of stress hormones has downstream effects on the neural architecture of the brain’s cognitive and emotional circuits.
Together, all of this evidence points to the urgent need of a solution to rectify these disparities.
Cultural competency stands out as a powerful tool for combating systemic racism, but understanding its true potential requires delving deeper into the construct of mental disorder diagnoses. Take for instance, the disease of schizophrenia. According to the Diagnostic and Statistical Manual, considered by many to be the bible of psychiatric diagnosis, the following criterion are needed to make a diagnosis of schizophrenia:
Notably absent from this definition is any mention of the culture and the context, a misstep with deadly consequences. A culturally competent approach recognizes the influence of culture and politics in defining what is considered pathology. As Alvin Pouissant, a clinical professor of psychiatry at Harvard Medical School, astutely notes,
This very issue unfolds within the definition of schizophrenia. Consider the case of a delusion, defined by the DSM-5 as “fixed beliefs that are not amenable to change in light of conflicting evidence.” Let’s imagine a patient expressing the belief ‘I don’t want to die like Trayvon Martin.’, I encountered such a scenario during my own psychiatry training. Would this qualify as a delusion? Here, a clinician must make a judgment call.
Perhaps a clinician deems it a delusion because no amount of reassurance can convince the patient that this outcome won’t occur. But what if the patient is Black, residing in a neighborhood where death by police is tragically not an uncommon occurrence? Does this perspective still qualify as a delusion? The answer to whether this belief constitutes a delusion begins to shift dramatically.
Thus, there is no denying that cultural context and cultural competence play a pivotal role in distinguishing a delusion from a patient’s lived experience and making an appropriate diagnosis. The very fabric of our diagnostic framework must recognize and account for the influence of culture to ensure that we don’t pathologize genuine reflections of an individual’s reality. By embracing cultural competency, we can dismantle the barriers that hinder accurate diagnoses and ensure that mental health care truly acknowledges and respects the diverse experiences of those we aim to support.
How then can we adequately incorporate culture into our diagnostic framework?
By implementing these strategies, we can foster a diagnostic framework that respects and incorporates culture as a vital aspect of mental health assessment. Ultimately, our goal should be to move away from a one-size-fits-all approach and embrace a culturally nuanced understanding of mental health, ensuring that diagnoses reflect the true experiences of individuals from diverse backgrounds. Through this transformation, we can establish a mental health care system that is equitable, inclusive, and responsive to the needs of all.
On May 1, 2023, Jordan Neely, a poor Black man, tragically lost his life on a New York subway train. A court of law will determine whether Daniel Penny should be held legally responsible for his death. Yet, beyond the trial, a haunting truth persists—Jordan Neely was already dead long before he stepped onto that train. Navigating the trauma of repeated encounters with the criminal justice system, mourning the loss of his mother who tragically and eerily died from strangulation, and disregarded by numerous bystanders, Neely’s death was the culmination of societal neglect and the absence of cultural understanding.
We all face a choice—actively prevent the mental decline of individuals like Jordan Neely or passively contribute to their suffering. Jordan Neely should still be alive today, reminding us of the imperative to address anti-Black racism in mental health care. We must take a stand against the pervasive biases and injustices that perpetuate these tragedies. In doing so, we can forge a path towards healing and a mental health care system that upholds the dignity, equality, and well-being of all individuals, regardless of their race or background. The choice is ours, and the time for change is now.
The mission of the Boston Congress of Public Health Thought Leadership for Public Health Fellowship (BCPH Fellowship) seeks to:
It is guided by an overall vision to provide a platform, training, and support network for the next generation of public health thought leaders and public scholars to explore and grow their voice.