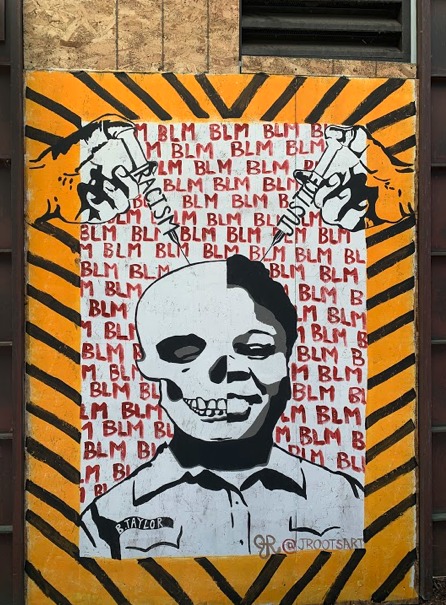
Sometimes racism kills quickly and violently – with whips, nooses and lynchings, chokeholds, carotid restraints, and shootings of unarmed Black people by police. Other times death by racism is – “death by 1000 cuts”– a slow, long, and drawn-out process. – akin to the brutal lingchi method of execution.
This is precisely what happens in Alzheimer’s Disease. In the initial stages, abnormal proteins accumulate inconspicuously in the background of any given neuron, silently corroding the mind as well as neural architecture. Eventually, years later, the protein reaches a critical threshold, setting off a neural chain reaction that leads to actual clinical and neurological symptoms. The first clinical symptoms may be subtle changes in memory, which then progress to distortions of cherished moments, personal history, and the loss of recognition of loved ones. In the final stages, even one’s own identity may be lost.
Jessica, an AD caregiver, eloquently captures the profound impact of this disease: “To be a caregiver of someone living with Alzheimer’s is that you watch your loved one die every day.”
However, the story does not end there. As racism can further compound this already challenging process in a multitude of ways. According to Carl V. Harris, chief diversity, equity, and inclusion officer at the Alzheimer’s Association, “Racism is trauma that can lead to increased stress…[and] can result in negative biological changes such as inflammation, a known risk factor for cognitive difficulties including dementia.” Although racism may not be the direct cause of dementia, its cumulative impact can be likened to the lingchi method, where a series of seemingly inconsequential injuries culminate in a fatal wound.
Just as the lingchi method inflicts numerous small cuts that eventually lead to death, the insidious effects of racism inflicts numerous small cuts on cognitive health over time. Structural racism, manifesting through factors, such as the cut of lower socioeconomic status, the slice of subpar early-life education, and the slash of a limited access to vital resources such as nutritious food and adequate healthcare, can contribute to inequities. These disparities, both individually and cumulatively impact the biological processes that elevate the risk of dementia over a lifetime.
Each act of discrimination and inequality (i.e. 1 of the thousand cuts), be it overt or subtle, adds to the burden carried by marginalized communities. These ongoing experiences of racism generate chronic stress, which, in turn, triggers a cascade of physiological responses that harm the body and brain. The resulting inflammation, oxidative stress, and other biological changes further exacerbate the risk of cognitive decline and dementia.
In short, Alzheimer’s disease is undoubtedly a devastating disease. Even more so for Black and other marginalized communities.
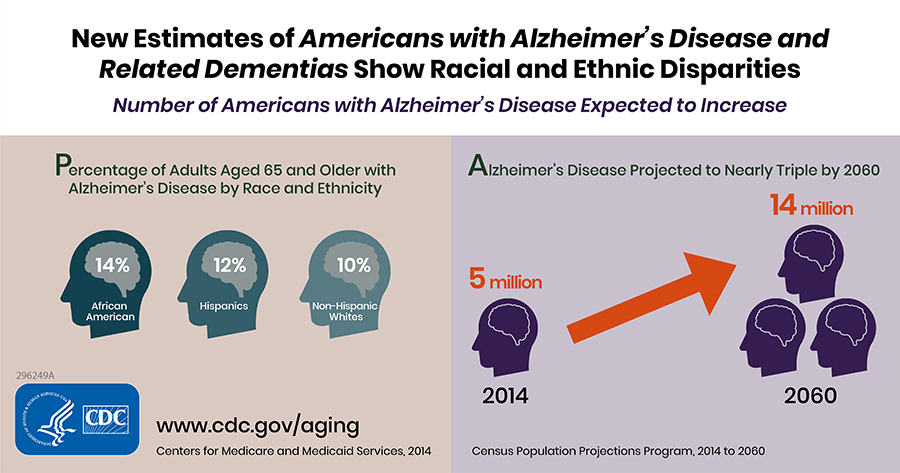
Today, an estimated 6.7 million Americans age 65 and older are living with Alzheimer’s Disease, and by 2060, it is projected this number will double, reaching an estimated 14 million individuals who suffer from Alzheimer’s Disease and related dementias. The toll is especially heavy for African Americans as accumulating evidence reveals a disturbing trend